Imagine suddenly developing confusion, memory problems, or hallucinations—frightening symptoms that might easily be mistaken for the onset of a severe psychiatric condition. In many cases, such individuals are diagnosed with conditions like schizophrenia and begin treatment accordingly. However, for some, the true cause lies elsewhere.
Take the case reported by Ford et al in 2019:
At 40 years old, a woman with no history of mental illness was suddenly no longer herself. Her family noticed confusion, forgetfulness, and strange behaviour. After being sent home from work for struggling with basic tasks, she grew increasingly disoriented and paranoid. When she was taken to the emergency department, she was labelled as having a drug-induced psychotic episode—her only positive result was for cannabis.
Despite days of treatment with antipsychotic medications, her condition deteriorated. She became non-verbal, suffered autonomic instability, and exhibited seizure-like activity. Only then did doctors begin to suspect something more than a psychiatric illness. Testing revealed N-Methyl-D-Aspartate receptor antibody-mediated (NMDAR) encephalitis– an autoimmune condition in which the body attacks the brain.
Her recovery took months and involved IVIG, steroids, plasma exchange, and intensive care. She gradually regained speech and cognition and was eventually discharged home with support. Five months later, she returned to work—almost back to baseline. Her story is a powerful reminder of how early diagnosis can change a life.
NMDAR encephalitis occurs when the body’s immune system mistakenly produces antibodies that attack NMDA receptors in the brain—receptors crucial for learning, memory, and synaptic communication. This immune attack leads to a disruption in normal brain function and triggers a wide range of symptoms, from psychosis and behavioral changes to seizures, movement disorders, and autonomic dysfunction. Because the initial presentation is often dominated by psychiatric symptoms, the condition is frequently misdiagnosed as a primary psychiatric disorder such as schizophrenia, especially in the early stages.
This misdiagnosis can delay appropriate treatment and expose patients to medications that not only fail to help but may also cause harm. While certain neurological symptoms—like seizures and orolingual dyskinesia—are less common in schizophrenia and may help flag the condition, research by Kayser et al. (2014) shows that approximately 4% of NMDAR encephalitis cases present with psychiatric symptoms alone, making diagnosis even more difficult.
Despite its severity, NMDAR encephalitis has a promising prognosis: more than 75% of patients experience substantial recovery when diagnosed and treated promptly with immunotherapy. Early identification is, therefore, critical—not just for reducing risk of long-term cognitive impairment, but for avoiding unnecessary distress, stigma, and inappropriate treatment pathways.
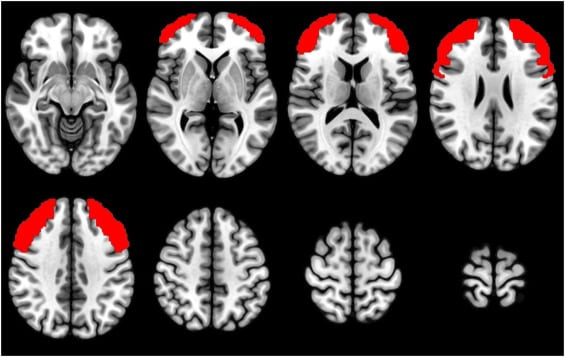
Our recent study, published in Psychiatry Research: Neuroimaging, set out to explore whether cognitive testing and brain imaging could help distinguish NMDAR encephalitis from schizophrenia (Kelleher et al, 2025). We compared three groups: Patients who had been diagnosed with and treated for NMDAR encephalitis, individuals with schizophrenia, and healthy controls. In addition to a comprehensive battery of cognitive tests, participants completed the N-back task—a computer-based task that measures short-term memory and attention—while undergoing fMRI brain scanning.
Previous meta-analyses (e.g., Glahn et al., 2005) have shown that schizophrenia is associated with reduced activation in the dorsolateral prefrontal cortex during the N-back task. However, to our knowledge, this is the first study to directly compare neural activation during this task in patients with NMDAR encephalitis with patients with schizophrenia and healthy controls.
Our findings were encouraging. Although patients with NMDAR encephalitis showed a trend toward slightly lower performance in several cognitive domains compared with healthy controls, and a trend toward higher performance in these same domains compared with patients with schizophrenia, none of the differences reached statistical significance. This suggests that, over time, cognitive function in individuals with NMDAR encephalitis may return to near-normal levels, particularly when early and effective treatment is administered.
These comparative data are reassuring and offer important clinical insights. They suggest that many patients can expect relatively favourable cognitive outcomes in the medium to long term, which may help clinicians when advising patients and their families after diagnosis. The evidence supports a hopeful message: substantial cognitive recovery is not only possible but likely, given appropriate and timely intervention.
At the same time, these findings underscore the urgent need for healthcare professionals to remain vigilant for the signs of autoimmune encephalitis in patients presenting with first-episode psychosis. Timely recognition and diagnosis are critical—not only for initiating appropriate immunotherapy but also for avoiding misdiagnosis and the long-term consequences of untreated brain inflammation. Early and accurate identification can preserve cognitive function, guide more effective treatment plans, and prevent patients from being misdirected into psychiatric care pathways that do not address the underlying cause of their symptoms. Indeed, early detection doesn’t just improve outcomes—it can give someone their life back.
References
· Ford B, McDonald A, Srinivasan S. Anti-NMDA receptor encephalitis: a case study and illness overview. Drugs Context. 2019 Aug 30;8:212589. doi: 10.7573/dic.212589. PMID: 31516531; PMCID: PMC6726359
· Glahn DC, Ragland JD, Abramoff A, Barrett J, Laird AR, Bearden CE, Velligan DI. Beyond hypofrontality: a quantitative meta-analysis of functional neuroimaging studies of working memory in schizophrenia. Hum Brain Mapp. 2005 May;25(1):60-9. doi: 10.1002/hbm.20138. PMID: 15846819; PMCID: PMC6871703.
· Kayser MS, Titulaer MJ, Gresa-Arribas N, Dalmau J. Frequency and characteristics of isolated psychiatric episodes in anti–N-methyl-d-aspartate receptor encephalitis. JAMA Neurol. 2013 Sep 1;70(9):1133-9. doi: 10.1001/jamaneurol.2013.3216. PMID: 23877059; PMCID: PMC3809325.
· Kelleher E, Mothersill D, Hargreaves A, Barry H, Smyth S, Chaila E, Boers P, McCabe DJH, Sweeney B, Costello D, Murphy KC, Cotter D, Doherty CP, Donohoe G, Corvin A (2025). Cognitive outcomes and performance of patients diagnosed and treated for N-Methyl-D-Aspartate receptor antibody-mediated (NMDAR) encephalitis compared with patients with schizophrenia and healthy controls,Psychiatry Research:Neuroimaging, Volume 349,111983,